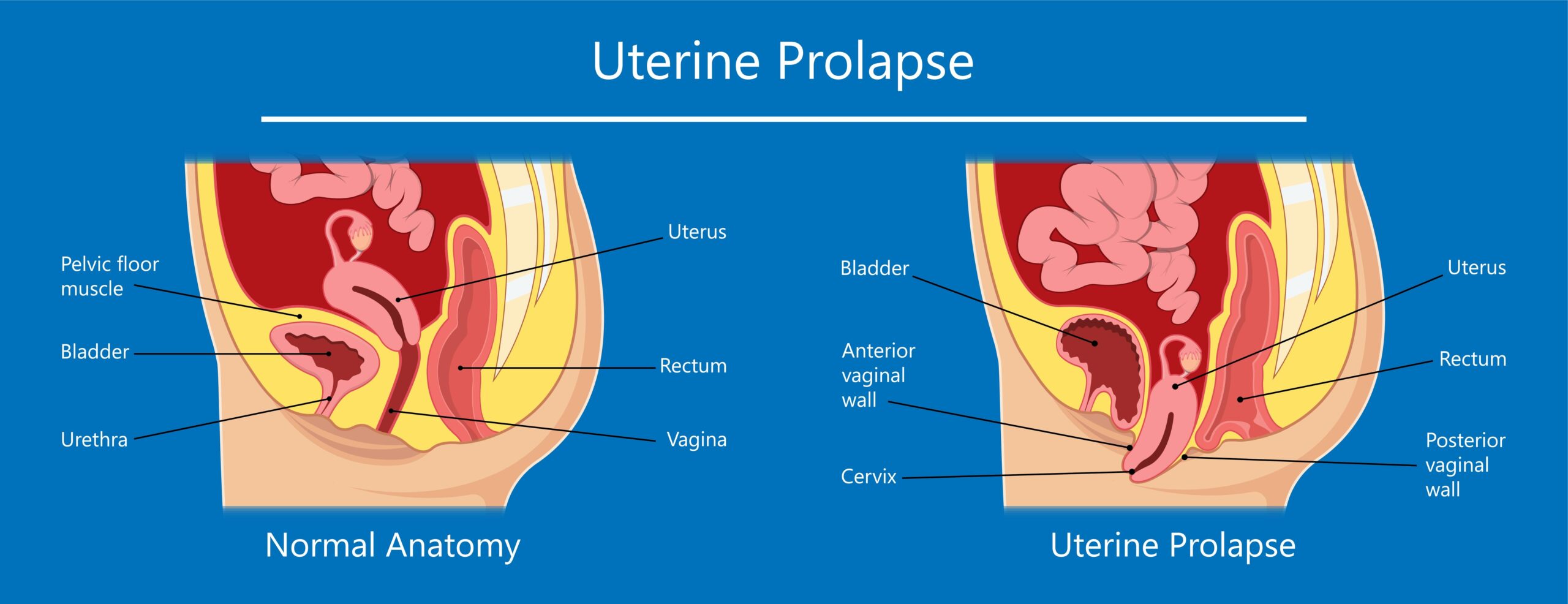
Pelvic organ prolapse (POP) is a condition that occurs when one or more pelvic organs, such as the uterus, bladder, or rectum, descend or shift from their normal positions and bulge into or outside the vaginal canal. This can happen due to weakened pelvic floor muscles and supportive tissues, which can no longer adequately support the organs. POP can cause discomfort, pain, and disruption of normal bodily functions. There are different types of POP, depending on which organ is affected:
Types of Pelvic Organ Prolapse:
Cystocele: This involves the bladder protruding into the front vaginal wall. It’s also known as a bladder prolapse.
Rectocele: This occurs when the rectum bulges into the back vaginal wall.
Uterine Prolapse: The uterus descends into the vaginal canal. This is more common in women who have given birth.
Vaginal Vault Prolapse: This type involves the top of the vagina sagging into the vaginal canal after a hysterectomy.
Enterocele: The small intestine presses against the vaginal wall.
Causes and Risk Factors:
Pelvic organ prolapse is often caused by weakened pelvic floor muscles and connective tissues, which can be due to several factors:
Pregnancy and Childbirth: The stress of pregnancy and vaginal childbirth can weaken pelvic floor muscles.
Aging: As women age, the supportive tissues in the pelvic area can naturally weaken.
Hysterectomy: Surgical removal of the uterus can alter the pelvic support structures.
Obesity: Excess body weight can strain the pelvic floor.
Chronic Constipation: Straining during bowel movements can weaken pelvic muscles.
Chronic Coughing: Conditions like chronic obstructive pulmonary disease (COPD) can cause frequent coughing, leading to POP.
Genetic Factors: Some women may have a genetic predisposition to weakened pelvic structures.
Symptoms:
Symptoms of pelvic organ prolapse can vary depending on the type and severity of the prolapse, but they may include:
A feeling of fullness or pressure in the pelvic area.
The sensation of a bulge or lump in the vaginal area.
Discomfort or pain during sexual intercourse.
Urinary issues such as leakage, frequent urination, or difficulty emptying the bladder.
Bowel issues such as constipation, difficulty emptying the bowels, or fecal incontinence.
Back pain or discomfort.
Treatment For Pelvic Organ Prolapse:
Treatment for pelvic organ prolapse depends on the severity of symptoms, the type of prolapse, and the patient’s preferences:
Lifestyle Changes: Maintaining a healthy weight, avoiding heavy lifting, and practicing proper bowel habits can help manage symptoms.
Pelvic Floor Exercises: Kegel exercises can strengthen the pelvic floor muscles and improve support.
Pessaries: These are medical devices inserted into the vagina to provide support for the prolapsed organ.
Physical Therapy: Pelvic floor physical therapy can provide exercises and techniques to strengthen pelvic muscles and alleviate symptoms.
Surgery: Surgical options include procedures to repair and reinforce the pelvic floor and prolapsed organs.
It’s important to consult a healthcare provider if you suspect you have pelvic organ prolapse. They can diagnose the condition, determine its severity, and recommend appropriate treatment options tailored to your individual needs.


