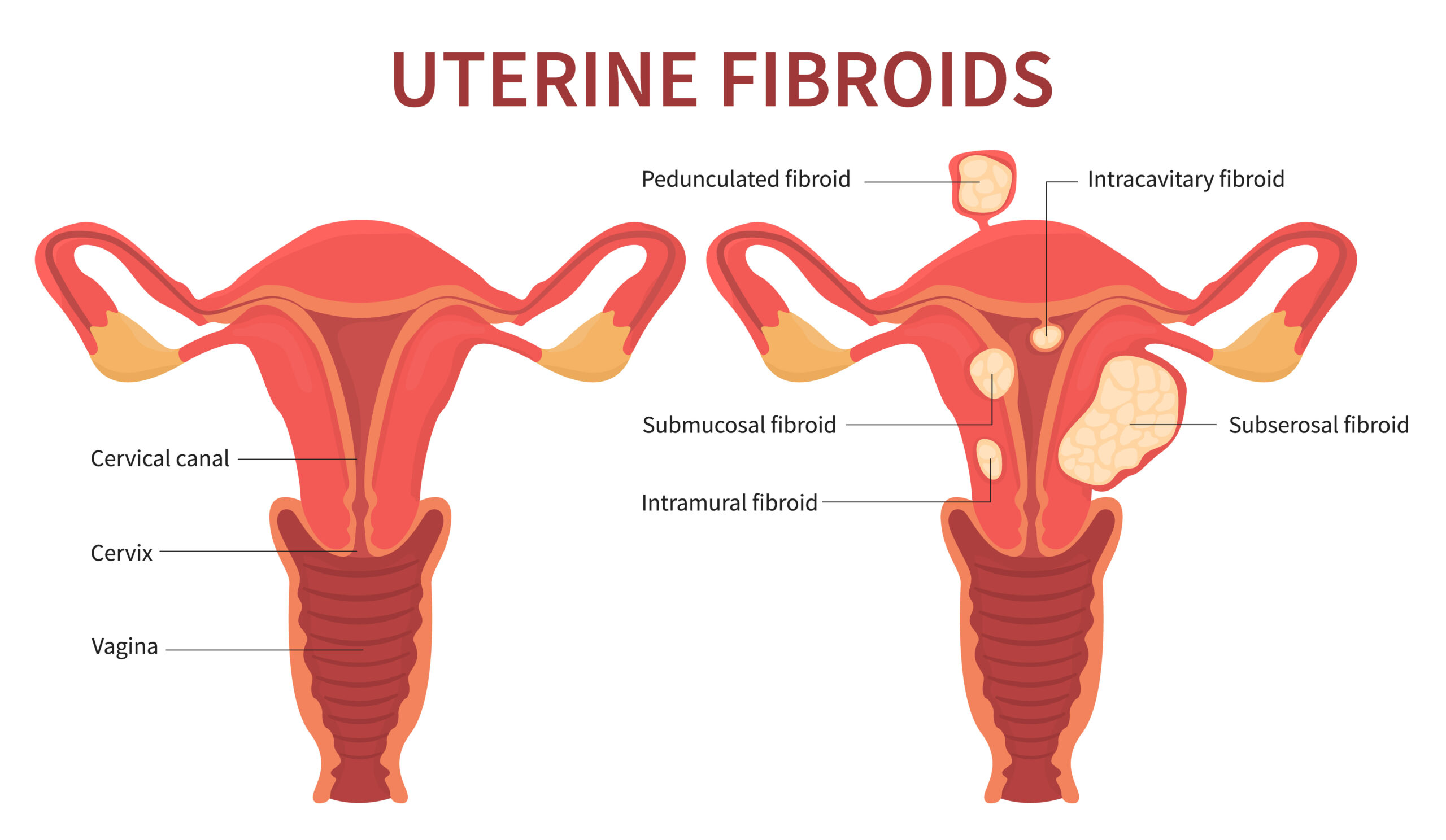
Uterine fibroids, also known as leiomyomas or myomas, are non-cancerous growths that develop in the uterus. They are made up of muscle and fibrous tissue and can vary in size, ranging from tiny, undetectable nodules to larger masses that can distort the shape of the uterus. Uterine fibroids are a common condition, particularly among women of reproductive age. Here’s what you need to know about uterine fibroids:
Causes and Risk Factors:
The exact cause of uterine fibroids is not fully understood, but various factors can contribute to their development:
Hormones: Estrogen and progesterone, the hormones that regulate the menstrual cycle, appear to play a role in the growth of fibroids.
Genetics: A family history of fibroids can increase the likelihood of developing them.
Age and Hormonal Changes: Fibroids tend to develop during the reproductive years and can shrink after menopause when hormone levels decline.
Ethnicity: Some ethnic groups, particularly African-American women, are at a higher risk of developing fibroids.
Symptoms of Uterine Fibroids:
Many women with uterine fibroids may not experience any symptoms, but when symptoms do occur, they can include:
Heavy Menstrual Bleeding: Excessive or prolonged menstrual bleeding is a common symptom.
Pelvic Pain and Pressure: Fibroids can cause pelvic discomfort, pressure, or a feeling of fullness.
Frequent Urination: Large fibroids can press against the bladder, leading to increased urination.
Pain during Intercourse: Fibroids can cause pain or discomfort during sexual activity.
Abdominal Swelling: Enlarged fibroids may lead to a noticeable increase in abdominal size.
Changes in Menstrual Patterns: Irregular periods, spotting between periods, or prolonged menstrual cycles can occur.
Diagnosis and Treatment:
Pelvic Examination: A healthcare provider may detect fibroids during a routine pelvic examination.
Ultrasound: Imaging tests like ultrasound can help visualize the size, location, and number of fibroids.
MRI: Magnetic resonance imaging (MRI) provides detailed images of fibroids and surrounding structures.
Biopsy: Rarely, a biopsy may be performed to rule out the presence of cancer.
Treatment Options For Uterine Fibroids:
Treatment for uterine fibroids depends on the severity of symptoms, the size and location of the fibroids, and the patient’s reproductive plans. Options include:
Watchful Waiting: If fibroids are small and not causing symptoms, a healthcare provider may recommend monitoring without treatment.
Medications:
Pain Relievers: Over-the-counter pain relievers can help manage pain and discomfort.
Hormonal Therapy: Hormonal medications like birth control pills, progestins, or GnRH agonists can regulate menstrual bleeding and alleviate symptoms.
Ulipristal Acetate: A selective progesterone receptor modulator that can shrink fibroids and alleviate symptoms.
Minimally Invasive Procedures:
Uterine Artery Embolization (UAE): This procedure cuts off the blood supply to fibroids, causing them to shrink.
Myomectomy: Surgical removal of fibroids while preserving the uterus, which can be done via laparoscopy, hysteroscopy, or open surgery.
Hysterectomy: In cases of severe symptoms or when fertility is not a concern, surgical removal of the uterus may be recommended.
Focused Ultrasound: This non-invasive procedure uses high-frequency ultrasound waves to heat and destroy fibroid tissue.
Lifestyle Modifications: Healthy lifestyle changes, including maintaining a balanced diet, managing weight, and staying active, can help alleviate symptoms.
It’s important to discuss your symptoms and treatment preferences with a healthcare provider. They can provide personalized recommendations based on your individual situation, helping you make informed decisions about managing uterine fibroids effectively.


